Introduction
Dental implant placement and implant-supported rehabilitations are extremely profitable remedy choices, and extra implants are being positioned lately by common dental practitioners and specialists than ever earlier than.1 For dental implant remedy to achieve success, it’s crucial to have a agency and secure osseointegration. The place, osseointegration is outlined because the direct structural and useful connection on the interface between bone tissue and the dental implant floor.2 Due to this fact, bone formation, transforming and metabolism performs an important position within the success of osseointegration.2,3 Aberrant bone metabolism has been proven to have a damaging impression on osseointegration which may end up in implant failure.3 Implant failures may be categorized as both early failure, which happen earlier than the prosthesis is positioned, and late failures, that are related to useful loading following placement of the prosthesis.4 Early failures regularly happen due to a disruption through the preliminary therapeutic part post-implantation, resulting in impaired bone-to-implant contact and the next failure of osseointegration;5 the onset of late failures could also be associated to a number of variables resembling peri-implantitis,6 systemic elements,7,8 overloading,9 and/or parafunctional habits.7,9,10
Bone metabolism is considered affected by a number of elements thus interfering with the standard of osseointegration.3 The prevalence of systemic illnesses and the associated consumption of medicines has elevated because the inhabitants ages. The consumption of medicines prescribed for some systemic illnesses and situations may probably modulate bone metabolism and negatively affect implant-related outcomes with an elevated threat of breakdown of the peri-implant tissues.11 Right here we briefly talk about two such drugs that are the Proton pump inhibitors (PPIs) and Selective serotonin reuptake inhibitors (SSRIs), and produce to the discover of our friends their potential affiliation with dental implant failures.
Proton pump inhibitors (PPIs) are a gaggle of medication which might be quickly turning into the third most prescribed pharmaceutical merchandise worldwide.12 PPIs are very efficient in each prevention and remedy of gastrointestinal acid associated situations, resembling peptic ulceration, gastroesophageal reflux illness (GERD or GORD), dyspepsia, helicobacter pylori infections, stress gastritis and eosinophilic esophagitis.13 PPIs irreversibly inhibit the proton pump within the acid-secreting parietal cells of the abdomen and thereby suppress the gastric acidity.14 PPIs supress gastric acidity by inhibiting the capabilities of the proton pump (H1/K1 ATPase),14 which may also be present in bone tissue.15 The proton pump inhibition of the osteoclasts can lower their actions and PPIs additionally impair calcium uptake by means of the intestines.16
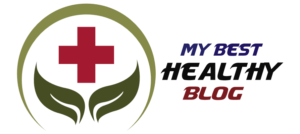
A number of observational research have proven an affiliation between the usage of PPIs and excessive threat of bone loss and bone fractures.17 Additionally, animal research have proven that PPIs administration in vivo can impair bone therapeutic and implant osseointegration 18. Inside the proof out there, systematic evaluations have confirmed an affiliation of PPIs with an elevated dental implant failure.19 There is a rise in sufferers which have had efficiently osseointegrated dental implant which were in perform and are failing after they’re prescribed PPIs (Fig. 1). Regardless of the identified damaging results of PPIs on the skeleton, the impact of those medicine has but not been completely explored in lots of vital bone-related medical situations together with osseointegrated dental implants. Many sufferers present process implant remedy are already taking PPIs with out a lot thought given to their potential impact on osseointegrated/osseointegrating dental implants.
Fig. 1
1A. Sinus raise process carried out for #2.6 implant web site preparation for a 55-year-old feminine affected person (August 2016). 1B. Implant positioned
at #2.6 web site (March 2017). 1C. Implant stage II process carried out (June 2017). 1D. Implant #2.6 restored (November 2017).
1E. Comply with-up appointment and continued upkeep remedy with no points (November 2018). In 2019, the affected person had a flare up of Irritable-Bowel-Syndrome (IBS) and was prescribed Pentaprazole (PPI) and Pinaverium Bromide. 1F. The implant was unfastened and there was lack of osseointegration (March 2021). 1G. The implant was misplaced because it fell out (April 2022)
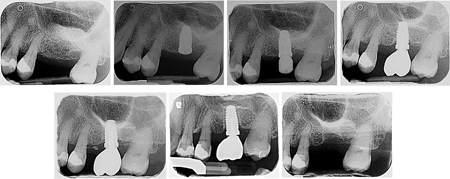
Selective serotonin reuptake inhibitors (SSRIs) are prescribed for the remedy and/or administration of depressive, or anxiousness situations. We’re seeing a serious improve in sufferers taking these drugs. There’s proof which factors in the direction of an affiliation of SSRIs with elevated dental implant failure charge19. We see in our medical observe an increasing number of sufferers who’ve been positioned on SSRI remedy after the implants have been loaded a couple of years again and are actually demonstrating peri-implant bone loss (Fig. 2). Current proof means that SSRIs have been recognized in enjoying a pivotal position on the osteoblast/osteoclast steadiness. Serotonin can regulate osteoclast activation and differentiation as osteoclasts derive from hematopoietic cell precursors.20 Moreover, SSRIs have been proven to supply a detrimental impact on bone mineral density and trabecular microarchitecture by means of their anti-anabolic skeletal results.21 Noteworthy, including to the impact on osteoclast activation, SSRIs might improve osteoclast differentiation and cut back osteogenic differentiation and mineralization, which can additionally negatively impression implant osseointegration. Lately, a preclinical in vivo examine has elucidated the impact of SSRIs on osteoblast differentiation and bone regeneration in rats.22 SSRI treatment considerably lowered osteogenic differentiation and mineralization with concomitant discount of osteoblast marker genes (together with alkaline phosphatase, Osterix, and osteocalcin), indicating its putative impression on the regulation of bone metabolism.22 Such mobile findings are in concordance with the outcomes obtained by Wu et al. (2014), who demonstrated that sufferers taking SSRIs skilled an elevated threat of dental implant failure.23
Fig. 2

2A. A Pre-operative radiograph of a 57-year-old male affected person, non-smoker, with non-contributory medical historical past, presenting with a circumferential bone defect round an implant #3.5 that had been loaded for two years. The affected person was positioned on Escitalopram (SSRI) 20 mg/day, one 12 months after the implant was loaded. 2B. The crown was eliminated, and a therapeutic screw was positioned till partial smooth tissue protection was achieved. Suppuration was evident upon compression. 2C. Upon full thickness flap elevation and thorough debridement of the defect, angular bone loss sample is noticed across the implant. 2D. The implant floor was rubbed with a cotton pellet soaked in 0.12% chlorhexidine for 1 minute, adopted by thorough rinsing with sterile saline. A contour strategy was used to regenerate the bone defect; first, autogenous bone chips have been harvested from a close-by space and packed throughout the defect. 2E. The autogenous bone chips have been overlaid with deproteinized bovine bone matrix (DBBM) xenograft, and a non-crosslinked collagen membrane was positioned over the implant. 2F. The flap was sutured in an effort to attain full, passive protection of the implant. 2G. The implant was uncovered at seven months; good high quality of the smooth tissues is seen, regardless of less-than-ideal plaque management within the adjoining dentition. 3 mm of keratinized tissue was preserved on the buccal facet with no bleeding on probing or suppuration across the implant. 2H. Seven-month post-operative radiograph previous to crown placement exhibiting full decision of the bone defect.
Current proof and findings from systematic evaluations present an affiliation of PPIs and SSRIs with elevated implant failure.19 The impact of those drugs requires additional investigation in future research as potential confounders for implant outcomes. A complete analysis and understanding of the affected person’s medical background and the medication-specific unintended effects on bone metabolism, is critical in assessing the affected person’s threat of implant issues when contemplating dental implant remedy. We advise discussing this with the affected person through the remedy strategy planning stage and being conscious of those implants having a lowered success charge.
Oral Well being welcomes this unique article.
References
- Gaviria, L., et al., Present tendencies in dental implants. 2014. 40(2): p. 50.
- Jokstad, A., Osseointegration and dental implants. 2009: John Wiley & Sons.
- Insua, A., et al., Foundation of bone metabolism round dental implants throughout osseointegration and peri‐implant bone loss. 2017. 105(7): p. 2075-2089.
- Moy, P.Ok., et al., Dental implant failure charges and related threat elements. 2005. 20(4).
- Baqain, Z.H., et al., Early dental implant failure: threat elements. 2012. 50(3): p. 239-243.
- Prathapachandran, J. and N.J.D.r.j. Suresh, Administration of peri-implantitis. 2012. 9(5): p. 516.
- Do, T.A., et al., Danger elements associated to late failure of dental implant—A scientific evaluate of latest research. 2020. 17(11): p. 3931.
- Paquette, D.W., N. Brodala, and R.C.J.D.C. Williams, Danger elements for endosseous dental implant failure. 2006. 50(3): p. 361-374.
- Sadowsky, S.J.J.I.j.o.i.d., Occlusal overload with dental implants: a evaluate. 2019. 5(1): p. 1-5.
- Chatzopoulos, G.S. and L.F.J.C. Wolff, Signs of temporomandibular dysfunction, self-reported bruxism, and the chance of implant failure: A retrospective evaluation. 2018.
- Aghaloo, T., et al., The Results of Systemic Illnesses and Drugs on Implant Osseointegration: A Systematic Assessment. 2019. 34.
- Mazer-Amirshahi, M., et al., Rising charges of proton pump inhibitor prescribing in US emergency departments. 2014. 32(6): p. 618-622.
- Metz, D.C.J.D., Potential makes use of of intravenous proton pump inhibitors to manage gastric acid secretion. 2000. 62(2-3): p. 73-81.
- Mullin, J.M., et al., Proton pump inhibitors: actions and reactions. 2009. 14(13-14): p. 647-660.
- Liu, J., et al., Proton pump inhibitors remedy and threat of bone illnesses: An replace meta-analysis. 2019. 218: p. 213-223.
- Wright, M.J., et al., Proton pump-inhibiting medicine, calcium homeostasis, and bone well being. 2008. 66(2): p. 103-108.
- Abrahamsen, B. and P.J.B. Vestergaard, Proton pump inhibitor use and fracture threat—impact modification by histamine H1 receptor blockade. Observational case–management examine utilizing Nationwide Prescription Information. 2013. 57(1): p. 269-271.
- Al Subaie, A., et al., Systemic administration of omeprazole interferes with bone therapeutic and implant osseointegration: an in vivo examine on rat tibiae. 2016. 43(2): p. 193-203.
- Chappuis, V., et al., Medicine-related dental implant failure: systematic evaluate and meta-analysis. 2018. 29: p. 55-68.
- Battaglino, R., et al., Serotonin regulates osteoclast differentiation by means of its transporter. 2004. 19(9): p. 1420-1431.
- Kahl, Ok.G., et al., Bone mineral density, bone turnover, and osteoprotegerin in depressed girls with and with out borderline persona dysfunction. 2006. 68(5): p. 669-674.
- Nam, S.S., et al., Serotonin inhibits osteoblast differentiation and bone regeneration in rats. 2016. 87(4): p. 461-469.
- Wu, X., et al., Proton pump inhibitors and the chance of osseointegrated dental implant failure: a cohort examine. 2017. 19(2): p. 222-232.
In regards to the Creator
 Dr. Zeeshan Sheikh is a Fellow of the Royal School of Dentist of Canada and Medical Scientist in Periodontics and Assistant Professor at Dalhousie College (departments of Utilized Oral Sciences, Dental Medical Sciences & Biomedical Engineering).
Dr. Zeeshan Sheikh is a Fellow of the Royal School of Dentist of Canada and Medical Scientist in Periodontics and Assistant Professor at Dalhousie College (departments of Utilized Oral Sciences, Dental Medical Sciences & Biomedical Engineering).
 Dr. Aditya Patel is a Fellow of the Royal School of Dentists of Canada and the present President of the Canadian Academy of Periodontology. He works in personal observe in Nova Scotia.
Dr. Aditya Patel is a Fellow of the Royal School of Dentists of Canada and the present President of the Canadian Academy of Periodontology. He works in personal observe in Nova Scotia.
 Dr. Eraldo L. Batista Jr. is a Fellow of the Royal School of Dentist of Canada and Affiliate Professor and Head of the Division of Periodontics at Dalhousie College, and Periodontist on the IWK Well being Centre.
Dr. Eraldo L. Batista Jr. is a Fellow of the Royal School of Dentist of Canada and Affiliate Professor and Head of the Division of Periodontics at Dalhousie College, and Periodontist on the IWK Well being Centre.